A well-known example of
multiple allele is the ABO blood grouping system in human. It was discovered by
Karl Landsteiner in 1901. An antigen is usually a foreign substance that enters
the body. Antibody is a protein that has been formed in response to antigen.
The red blood cells have antigen. The plasma has antibodies. Two antigens A and
B and corresponding antibodies have been distinguished. Sometimes clumping
occurs when red blood cells of one person are mixed with the blood plasma of
another person. On the basis of the reactions mankind are divided into four
groups, A, B, AB, O. Some people were found to have ‘A’ antigen some had B and
some had both A and B and some had neither A nor B antigen. Those with A type
blood did not carry the corresponding anti A antibody, but they did carry
anti-B in their plasma. B type people carry anti A but not B. Persons with AB
type blood have both A and B antigens associated with the red blood cells, but
no Anti A or Anti B antibodies in their plasma. O type individuals have no A
and B antigens but carry both anti A and Anti B antibodies in the plasma.
 |
| Multiple Alleles for the ABO blood group |
 |
| ABO BLOOD GROUP |
Agglutination
When two different
blood groups are mixed, antigen of one reacts with the antibodies (agglutinin
which acts as an antibody) of the other, then the RBC clump with one another.
The clumping of RBC is known as agglutination.
Genotype of ABO Blood Group
In 1925 Berstein
explained the genetic basis of ABO system. Blood group is controlled by
autosomal single polymorphic gene I on chromosome. The gene locus (place) is
represented by the symbol I (which stands for isohaemagglutinogen). There are
three alleles represented by the symbol A, B (these letters refer to two
carbohydrates designated A and B which are found on the surface of RBC) and i.
The alleles A and B are equally dominant so they are called co-dominant and i
is recessive to both A and B.
Example
The genotype I^i would
give rise to the agglutinogen A on the red blood cell membrane and the plasma
would contain agglutinin anti-B. The blood group would be A. Blood group A may
be homozygous AA and heterozygous Ai. Blood group B may be heterozygous Bi,
blood group AB is heterozygous AB (co-dominant). Blood group O is always
homozygous ii. The four blood groups do not change during the life time of any
human being.
Importance of blood group
Blood grouping is
important in:
(a) Transfusion
(b) Establishment of
paternity
Transfusion
If a person with blood
group A gives blood to a person with type B there will be clumping of blood due
to presence of anti A in the blood group B and the recipient will probably die.
A person with blood group AB has neither anti A nor anti B plasma antibody and
can safely receive A, B or O blood group. A person with blood group O has no
cell antigen and can safely give blood to any of the other type. The person
with blood group O is therefore known as a universal donor.
Explain
Using Appropriate Genetic Symbols The Possible Blood Groups Of Children Whose
Parents Are Both Heterozygous, The Father Being Blood Group A And The Mother B.
In the ABO blood group
system, there are four possible blood groups: A, B, AB, and O. These blood
groups are determined by the presence or absence of two types of antigens (A
and B) on the surface of red blood cells, and the presence or absence of
antibodies against these antigens in the plasma.
Let's represent the
blood group alleles using appropriate genetic symbols:
The blood group A
allele is represented as "IA".
The blood group B
allele is represented as "IB".
The blood group O
allele (which does not have any antigens) is represented as "i".
Given that the father
is blood group A and is heterozygous (IAi), and the mother is blood group B and
is also heterozygous (IBi), here are the possible blood groups of their
children using a Punnett square:
Father's
alleles: IAi
Mother's
alleles: IBi
Possible
combinations of alleles in the children:
IA
from father and IB from mother: The child will have
blood group AB (IAIB), as both A and B antigens are present on the red blood
cells.
IA from father and i
from mother: The child will have blood group A (IAi), as only A antigen is
present on the red blood cells.
IB
from father and IA from mother: The child will have
blood group AB (IAIB), as both A and B antigens are present on the red blood
cells.
IB
from father and i from mother: The child will have
blood group B (IBi), as only B antigen is present on the red blood cells.
Therefore, the possible
blood groups of the children of heterozygous parents, where the father is blood
group A and the mother is blood group B, can be AB, A, B, or AB, depending on
which alleles are inherited from the parents.
A
Woman With Blood Type B Has A Child With Blood Type O. What Are The Genotypes
Of The Mother And Child? Which Genotypes Could The Father Not Have?
Based on the given
information, we can deduce the possible genotypes of the mother and child, as
well as the genotypes that the father could not have.
Let's represent the
blood type alleles using appropriate genetic symbols:
The blood type A allele
is represented as "IA".
The blood type B allele
is represented as "IB".
The blood type O allele
(which does not have any antigens) is represented as "i".
Given that the woman
has blood type B, which means she has at least one "IB" allele, and
the child has blood type O, which means the child has two "i"
alleles, we can deduce the following:
Mother's
genotype: Since the woman has blood type B, she could have
two "IB" alleles (IBIB) or one "IB" allele and one
"i" allele (IBi) genotype.
Child's
genotype: Since the child has blood type O, which does not
have any antigens, the child must have two "i" alleles (ii) genotype.
Father's
possible genotypes: The father could not have blood type A,
as the child has blood type O which does not have any "A" antigens.
Therefore, the father must have either blood type B (IBIB or IBi genotype) or
blood type O (ii genotype).
In conclusion, the
possible genotypes for the mother could be IBIB or IBi, the child must have the
ii genotype, and the father could have either IBIB, IBi, or ii genotype.
Rh Blood Group
The Rh blood group was
named after the Rhesus monkey, in which it was first studied by Landsteiner in
1930’s. In humans this group includes antigens or factors called Rh factor. If
Rh factor is present in the red blood cell membranes, the blood is said to be
Rh positive and if the red blood cells lack Rh factor, the blood is called Rh
negative.
Genes of Rh factor
Rh blood group is
encoded by three genes C, D, and E. These genes occupy two tightly linked loci.
D occupy one locus called locus D. The genes C and E alternatively occupy other
loci. The most important of these is D locus.
Gene D
Gene D has two alleles,
D and d. Gene D is completely dominant over gene d. Persons having genotype DD
or Dd have Rh factor on their red blood cells and are Rh positive. Persons with
genotype dd do not have Rh factor and are Rh negative.
Antibody against Rh antigen
This antibody is not
present in the ABO blood groups. It is only formed when Rh antigen comes in
contact with A/B/AB/O blood groups. So the blood of the Rh negative person
contains neither Rh antigen on its cells or Rh antibody in plasma. If the Rh
negative person is given Rh positive blood, it will stimulate the plasma to
produce antibody. If the same Rh negative person is given Rh positive blood,
the antibody already formed in the plasma against Rh positive will react with
donated blood. The person can even die. So for the transfusion of the blood,
not only blood group A, AB, B, O is matched but the Rh factor is also matched
i.e. Rh positive blood can be given only to Rh positive person and Rh negative
blood can be given only to Rh negative person. So ABO blood group is written
as:
Erythroblastosis Fetalis
The Rh factor is
particularly important during pregnancy. Rh positive is dominant over Rh
negative. If the mother is Rh negative (dd) and father's genotype is DD, all
the offspring (Dd) will be Rh positive.
DD (Father) x dd
(mother) = Dd (child)
If the father is
heterozygous (Dd) the child has a fifty percent chance of being Rh positive.
Dd (father) x dd (mother)
= Dd, Dd, dd, dd (child)
The red blood cells of
an Rh+ child will leak across the placental barrier into the mother's
circulatory system because placental tissues normally break down before and at
birth. The presence of these Rh antigens causes the mother to produce anti- Rh
antibodies. In this or a subsequent pregnancy with an Rh-positive baby, anti-Rh
antibodies produced by the mother may cross the placenta and destroy this
child's red blood cells. This is called hemolytic disease of the now born or
erythroblastosis fetalis. This anemia may lead to abortion or still birth. Even
if the pregnancy continues, the liver and spleen of the fetus swell as they
rapidly produce red blood cells. The breakdown product is called bilirubin.
Haemolysis continues after the baby is born. Due to red blood cell destruction
followed by haeme breakdown, bilirubin rises in the blood. Excess bilirubin can
lead to brain damage, mental retardation, jaundice and even death.
 |
| Haemolytic disease of the new born |
Prevention:
The problem has been solved by giving Rh- negative women an Rh immunoglobin
injection either midway through the first pregnancy or no later than 72 hours
after giving birth to an Rh-positive child. This injection contains anti-Rh
antibodies that attack any of the baby's red blood cells in the mother's blood
before these cells stimulate her immune system to produce her own antibodies.
This injection is not beneficial if the woman has already begun to produce
antibodies; therefore, the timing of the injection is most important.
Test
of Rh factor: To test if an individual is Rh negative
or Rh positive blood is mixed with an anti Rh antibodies. When Rh-positive
blood is mixed with anti-Rh antibodies, agglutination occurs.
An
Rh negative woman is married to an Rh positive man whose father was also Rh
negative. What are the possible genotypes of each person in the family? What
are the chances that their child will be affected?
The Rh blood group
system is determined by the presence or absence of a protein called the Rh
factor on the surface of red blood cells. An individual who has the Rh factor
is considered Rh positive (Rh+), while an individual who lacks the Rh factor is
considered Rh negative (Rh-).
In this scenario, we
can use Punnett squares to determine the possible genotypes of each person in
the family. The possible genotypes for each person are:
RH
negative woman: RR or Rr
RH
positive man: Rr or RR (if his father is also Rh
negative, he must be heterozygous for the Rh factor)
Father
of RH positive man: rr
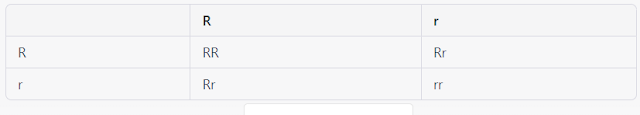
Using this information,
we can create a Punnett square to show the possible genotypes of their
offspring:
The chances that their
child will be affected (i.e., have Rh disease) depend on the genotype of the
parents. If both parents are Rh positive or both parents are Rh negative, their
child will not be affected. However, if the mother is Rh negative and the father
is Rh positive, there is a 50% chance that their child will inherit the
Rh-positive allele from the father, making the child Rh positive. If an
Rh-negative mother carries an Rh-positive baby, her immune system may recognise
the baby's Rh factor as foreign and produce antibodies to attack it. This can
lead to hemolytic disease of the newborn (HDN), a condition in which the
mother's antibodies attack and destroy the baby's red blood cells, causing
anaemia and other complications. To prevent HDN, Rh-negative mothers are
typically given a medication called Rh immunoglobulin during pregnancy and
after delivery if the baby is Rh positive.
A
man and his wife are both heterozygous for Rh positive. They have three
children; all of them are Rh negative. How is this explained? What are the
chances that their next child will be Rh positive or Rh negative?
In this scenario, both
the man and his wife are heterozygous for the Rh factor, which means they each
have one Rh-positive allele and one Rh-negative allele. The possible genotypes
for each parent are:
Man:
Rr (one Rh-positive allele and one Rh-negative allele)
Woman:
Rr (one Rh-positive allele and one Rh-negative allele)
When they have
children, the possible genotypes for each child are:
Rh-positive (RR or Rr)
Rh-negative (rr)
Using a Punnett square,
we can see that the probability of having an Rh-negative child when both
parents are heterozygous is 25%, and the probability of having an Rh-positive
child is 75%:
Therefore, it is
possible for a couple who are both heterozygous for the Rh factor to have
Rh-negative children.
The chances of their
next child being Rh positive or Rh negative will depend on the genotype of the
parents. Since both parents are heterozygous, there is a 25% chance that the
next child will be Rh-negative (rr), a 50% chance that the child will be
heterozygous like the parents (Rr), and a 25% chance that the child will be
Rh-positive (RR). It's important to note that each pregnancy is independent, so
the outcomes of previous pregnancies do not affect the chances of future
pregnancies.